Menu
Close
Major Depressive Disorder, Part One | Defining MDD and its impacts
Nov 9, 2022
This two-part series details the Canadian Mental Health Association (CMHA), Alberta Division’s three-year research project on Major Depressive Disorder (MDD); the impact MDD has on the lives of Canadians, how they cope with MDD, and what a brighter future looks like for Canadians with MDD – all through the lens of lived experience. In part one, how MDD manifests in the everyday lives of Canadians will be explored.
The MDD Project
Major Depressive Disorder is a type of depression that affects all Canadians in some way – whether it be personally, through family, or through someone they know. MDD is defined as depression that persists through the prescription of two or more antidepressants.
With MDD’s main descriptor being its persistence through medicative treatment, understanding how it affects Canadians is rooted in its treatment and impacts; how are Canadians with MDD affected by it, what are common methods for ongoing treatment, and what can be done to improve their lives?
Determining that lived experience research was the best way to get answers. CMHA, Alberta Division spent three years conducting surveys, one-on-one interviews, and a national, virtual townhall to get perspective from Canadians with MDD and people caring for them. This is what they said.
Impact
Symptoms
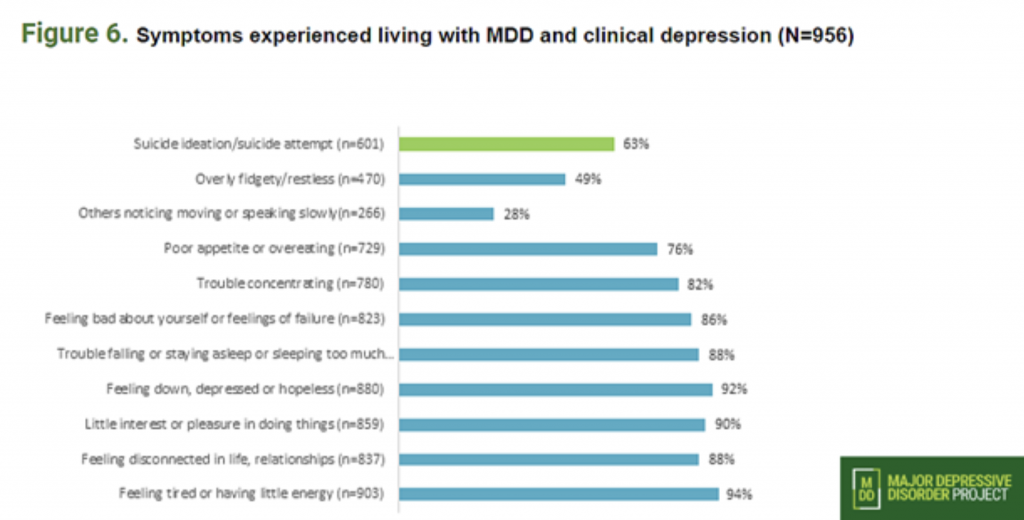
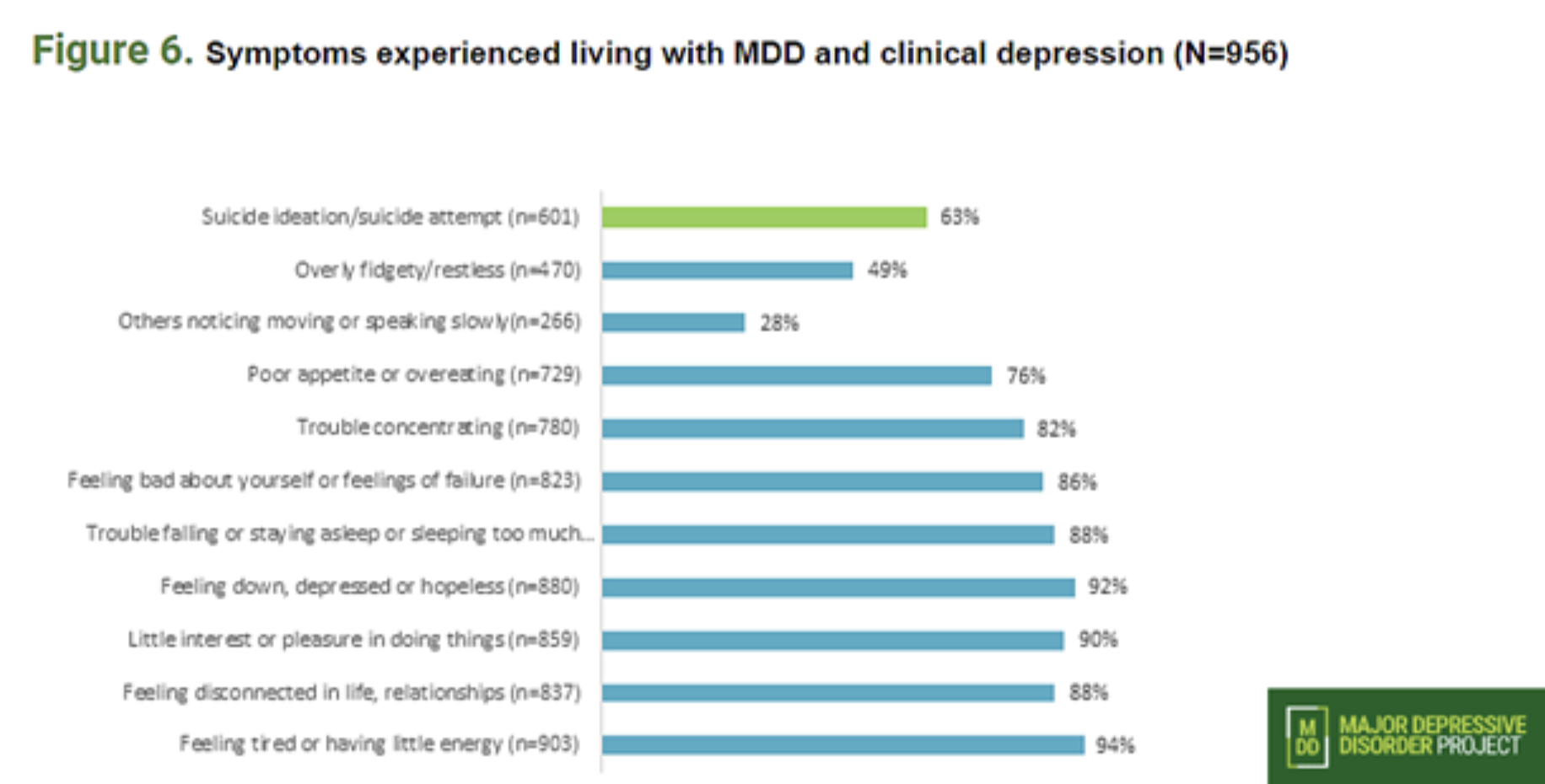
Depression affects everyone differently, manifesting in a wide array of symptoms. MDD’s most notable symptoms include feeling disconnected and down, feeling fatigued, difficulty sleeping or sleeping too much and suicidal thoughts. Some lesser-known symptoms that reflected strongly in surveys were appetite issues (eating too much or too little), fidgeting or lack of concentration, and persistent feelings of failure or self-judgment.
Relationships
One of the many challenges for those living with MDD is a general lack of energy. This struggle to maintain enthusiasm for daily activities or relationships can cause severe strain with family, friends and partners. 80 per cent of survey respondents stated these strains in personal relationships stemmed from both their own lack of motivation and the lack of understanding from people in their life for what they were experiencing.
Respondents cited this lack of understanding, compiled with general stigmatization of depression, as common problems with friends and family that often lead to hesitancy to disclose a diagnosis or reach out for help.
The Workplace
The stigmatization of MDD also plays a major role on Canadians’ professional lives. Living with MDD means fearing judgment or a change in treatment in a workplace setting upon disclosure of a diagnosis – or anxiety to even pursue a diagnosis in the first place. A staggering 46 per cent of survey respondents with MDD in the workplace had not disclosed their diagnosis to their employer.
While fear of disclosure limiting professional growth was a common experience amongst respondents, women, people who do not identify on the gender binary, and people who do not identify as white all felt higher apprehension about disclosing a diagnosis.
Covid
Across all research done by CMHA, Alberta Division, Covid has been cited as having a major effect on the day-to-day life of Canadians with MDD. At work and at home, the pandemic represented sweeping changes in how we do things and interact with each other.
The harm that increased isolation, disruption in work life or even job loss, pandemic anxiety and the restriction of vital care and services has done was echoed in many respondents’ comments: “Covid and other co-occurring crises have tested my resiliency and increased my health anxiety. Covid has changed routines that I relied upon for mental wellness and isolated me from my support network and friends.”
Increased isolation and restricted coping mechanisms have definitively exacerbated symptoms for Canadians living with MDD, and while the availability of online resources has grown as a result, many respondents voiced that the impact of these supports fell short of the in-person care they received prior to the pandemic.
Coping
The main avenues for coping with MDD are prescription medicine, professional support like doctors and psychiatrists, social support like friends and family, and healthy lifestyle choices. Some of the less prevalent answers by survey respondents included alcohol and cannabis.
Beyond affecting relationships and the workplace, more mundane areas of life may be a struggle for people living with MDD. Society’s understanding of the mental health benefits of proper self-care have come a long way, but these small acts of maintenance can prove difficult for a person with MDD.
What Does it All Mean?
CMHA, Alberta Division’s research helped define a clearer picture of how MDD symptoms manifest in Canadians, the impacts these effects can have on their lives, and the methods of coping that are most common. A better understanding of what daily life looks like for people living with MDD is vital to understanding what obstacles they face and how supports, policies and advocacy can begin to navigate a way forward.